Can PCOS cause liver problems, like fatty liver? The short answer: it’s complicated.
PCOS itself is the result of many underlying health abnormalities, including insulin resistance, stress, hypothyroidism, poor gut health, and inflammation.
It’s not exactly accurate to say PCOS causes liver problems. However, many of the underlying causes of PCOS can also lead to fatty liver. Research shows that women with PCOS have a higher risk of fatty liver (1). So, let’s dig in!
What is the liver? And what does it do for us?
The liver is a reddish-brown organ that sits on the upper right side of the abdominal area, right on top of the stomach, intestines, and the right kidney.
It weighs about 3 pounds and has many important functions, including:
- Storing nutrients, like iron, copper, Vitamin A, D, E, K, B12.
- Balancing blood sugar. The liver stores away sugar, when there is too much in the blood and releases sugar into the blood during fasting and stressful times.
- Activating thyroid hormone (T4 to T3 conversion).
- Neutralizing estrogen and sending it to the gut to be detoxified (aka pooped out).
- Making proteins that play a role in blood health, hormones, fat processing, etc.
- Making bile, which helps digest protein and fats.
- Neutralizes drugs and other toxic substances and redirects them to the gut or kidneys to be eliminated.
What is fatty liver?
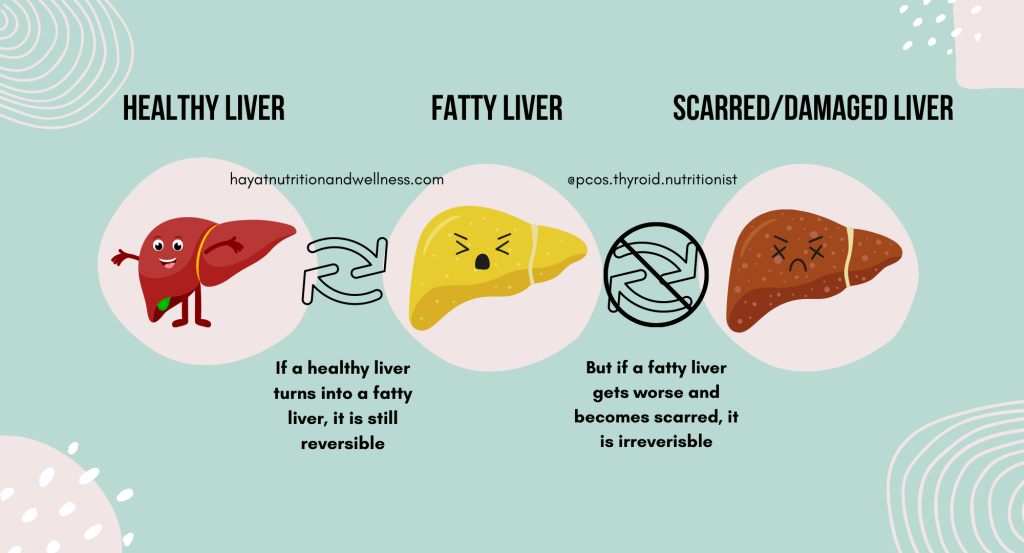
Fatty liver is also known as Non-Alcoholic Fatty Liver Disease (NAFLD) or steatosis. It’s exactly what it sounds like: too much fat stored in liver cells and inflammation of the liver, which isn’t caused by drinking alcohol. It can be mild, moderate, or severe.
The prevalence of fatty liver is increasing. In the US alone, 24% of adults have fatty liver and it’s the most common type of chronic liver disease.
It’s important to address fatty liver in its earlier stages when it’s reversible.
Fatty liver can worsen into nonalcoholic steatohepatitis (NASH) and lead to scar tissue forming in the liver. Scar tissue prevents proper functioning. Ultimately, this causes liver failure.
The risk factors for fatty liver overlap with characteristics of PCOS
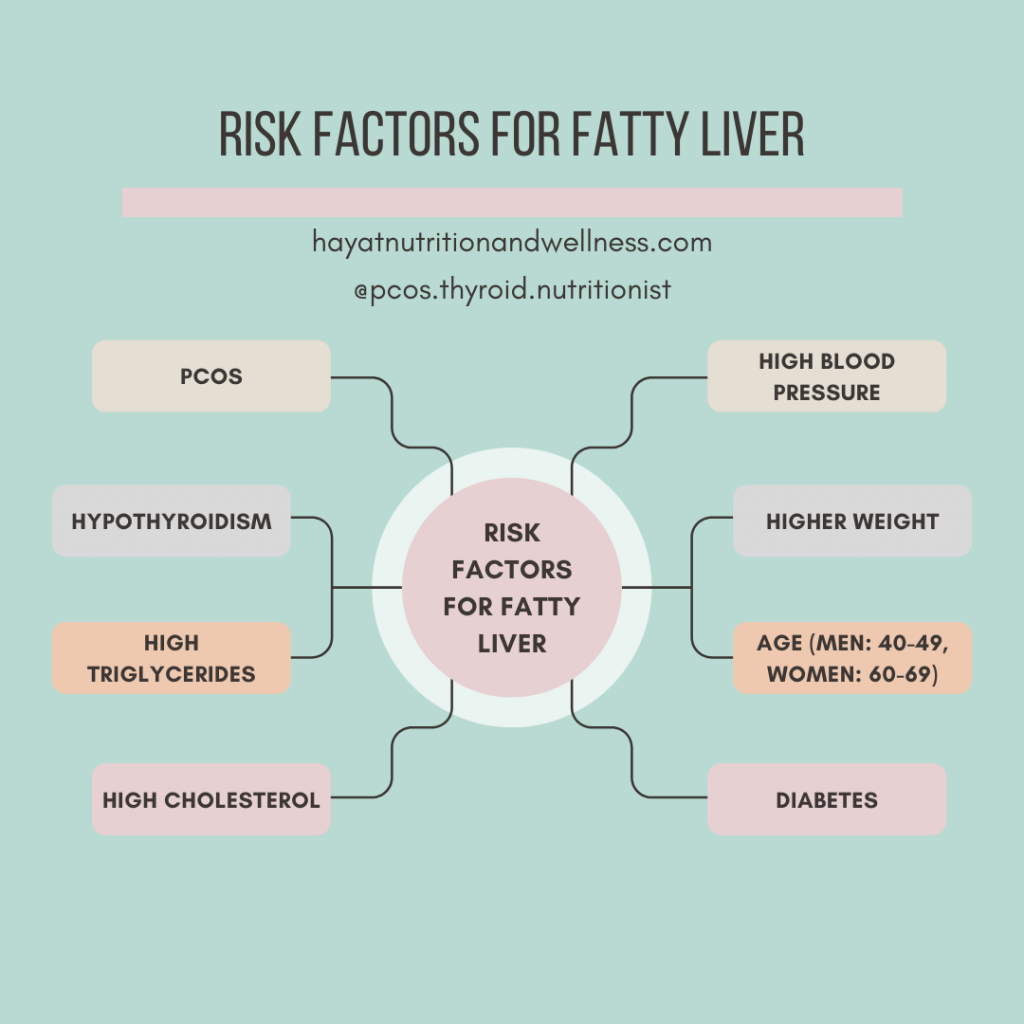
If you have any of the following conditions or fall into a specific age group, you may be at an increased risk for fatty liver.
- PCOS (polycystic ovary syndrome). I talk in more detail on whether PCOS can cause liver problems below.
- Hypothyroidism
- Diabetes
- Age. A 2013 study found that fatty liver increased with age. Men between 40-49 years had higher rates of fatty liver and women between 60-69 had higher rates (2).
- High cholesterol
- High triglycerides
- High blood pressure
- Higher weight
Characteristics of PCOS that are also risk factors for fatty liver
- High cholesterol
- High triglycerides
- Insulin resistance or higher risk for diabetes
- Underlying causes could be hypothyroidism
- Higher weight
Fatty liver doesn’t have many symptoms. How is it assessed?
Two symptoms that could indicate fatty liver are fatigue and abdominal pain in the upper right side. Since these symptoms aren’t very unique, it’s important to discuss with your doctor if you have any of the risk factors.
There are a couple ways your healthcare provider can check for fatty liver (3):
- A blood test to see if you have high liver enzyme levels, which can show inflammation in the liver.
- Ultrasound, MRI, or CT scan to visually see if the liver is healthy.
The 4 links between PCOS and fatty liver
So, back to the original question: can PCOS cause liver problems?

Insulin resistance or lowered ability to process sugar
What is insulin?
Insulin is a hormone that helps each of our cells absorb sugar or glucose. It’s released after we eat, from an organ called the pancreas. Insulin knocks on the door of each of our cells to tell them, “hey, there’s extra glucose in the blood, please take some.”
If everything is working as it should, the cells open their doors and take in sugar from the blood. Cells cannot take in sugar without insulin.
What is insulin resistance?
Insulin resistance occurs when cells cannot hear insulin knocking clearly anymore. If our cells cannot hear the knock, then they cannot open the door to let sugar in. This leaves too much sugar in the blood.
In response, the body produces more and more insulin so it can make a louder knock on the cell’s door to get sugar inside our cells. This can lead to high insulin levels in the blood (called hyperinsulinemia).
To learn more about insulin resistance in depth and how it plays a role in PCOS, check out my blog post “A Deep Dive into Insulin Resistance.”
The link between insulin resistance and fatty liver
When controlling for weight and diabetes, people with fatty liver are more likely to have insulin resistance or poor blood sugar regulation (4).
When cells are not able to hear the signal from insulin, they also can’t get the sugar they need to make energy. So they break down fat instead. Some of this fat is used in the cell to make energy, and some of it is sent into the blood and carried to the liver where it gets stored.
It’s important to remember that insulin resistance and fatty liver have a cyclical relationship. Fatty liver can also contribute to insulin resistance, just like insulin resistance contributes to fatty liver (5).
The link between insulin resistance and PCOS
65-70% of women with PCOS struggle with insulin resistance and high insulin levels. The likelihood that they have had blood sugar regulation issues long before their diagnosis is high.
Here’s why Insulin resistance plays a BIG role in PCOS (6):
- It increases male hormone production from the ovaries. This leads to symptoms like coarse, dark facial hair and male pattern baldness.
- Insulin resistance blocks the liver from producing sex hormone binding globulin (SHBG). SHBG is a protein found in the blood that binds testosterone and estrogen. Not having enough of this protein means there’s extra testosterone and estrogen in the body, which makes PCOS symptoms worse.
- It can cause weight gain or make it harder to lose weight. This causes excess estrogen to be made in the body, because fat tissue has a specific protein that can convert testosterone to estrogen. Too much estrogen, also known as estrogen dominance, is a big cause of PCOS symptoms. It’s also a part of a vicious cycle, where estrogen can make insulin resistance worse.
- Insulin resistance can lead to irregular ovulation, which can show up as: not having a period, having very long cycles (a few periods a year), or even menstruation without ovulation (called anovulatory cycles).
Higher weight
Carrying excess weight, especially in the midsection is a common characteristic of people with PCOS and fatty liver.
Research shows being at a higher weight can exacerbate PCOS symptoms and increase risk for fatty liver. This is not always the case. Lean PCOS and fatty liver is also possible. This points to the fact that excess weight is more likely a by-product of the underlying health abnormalities that cause PCOS and fatty liver than a contributing factor. Many chronic conditions are complex and interconnected. Being at a higher weight may increase your risk for fatty liver. AND the different components that increase risk for fatty liver also increase risk for excess weight (i.e. insulin resistance).
Poor gut health
You may have poor gut health if you have symptoms like constipation, on and off diarrhea, excess gas, bloating, insulin resistance, inability to lose weight, intolerance to certain foods (gluten, dairy), fatigue, headaches, skin problems (acne, eczema), arthritis, PCOS, fatty liver, etc.
Poor gut health happens when the good and bad bacteria are out of balance and there’s less diversity in the kind of bacteria and microorganisms in the gut. An imbalance in good and bad bacteria is called gut dysbiosis. Leaky gut (also known as high intestinal permeability) is another characteristic of poor gut health.
PCOS and fatty liver are both linked to gut dysbiosis and lower gut diversity (7). When compared to healthy individuals, people with fatty liver are also more likely to have leaky gut. Leaky gut leads to absorption of endotoxin, which causes inflammation and is linked to fatty liver. Endotoxin is a toxin produced by gram-negative bacteria in the gut, which takes a ride on fat to get into the blood and reach the liver. Endotoxin can cause inflammation and insulin resistance.
High male hormones
Excess male hormones are a key characteristic of PCOS. Excess male hormones cause unwanted coarse facial hair, male pattern baldness, and interrupt ovulation.
Research shows that high male hormones can contribute to fatty liver in people with PCOS by directly increasing fat accumulation in the liver, contributing to insulin resistance, and contributing to abdominal weight gain (8).
Summary
Fatty liver starts when too much fat begins to build up in liver cells and there is inflammation. It can progress to scarring of the liver and ultimately, liver failure. People with PCOS are more likely to get fatty liver, because many of the underlying causes of PCOS are also the underlying causes of fatty liver. These include insulin resistance, higher weight, poor gut health, and high male hormones.
Do you need support in navigating PCOS? Check out my guide, “I (may) have PCOS, now what?” HERE.
- Understand PCOS Sugar Cravings & How to Stop Them - March 24, 2023
- The 4 Types of PCOS – What You Need to Know - February 24, 2023
- 4 Reasons Not to Keto with Hypothyroidism - January 27, 2023